Cardiovascular mortality and microinflammation in abdominal obese hemodialysis patients
Srčnožilna umrljivost in mikrovnetje pri trebušno debelih hemodializnih bolnikih
DOI:
https://doi.org/10.18690/actabiomed.90Keywords:
microinflammation, inflammatory mediators, cardiovascular mortality, abdominal obesity, hemodialysisAbstract
Purpose: Abdominal adipose tissue has important inflammatory properties and is a source of various inflammatory mediators. Given that concentrations of some inflammatory mediators are high among hemodialysis (HD) patients, abdominal obesity may play an important role in the pathogenesis of microinflammation which is known to be associated with accelerated atherosclerosis. The aim of our study was to determine the impact of microinflammation on cardiovascular (CV) mortality in abdominal obese HD patients.
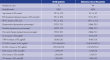
Methods: Seventy–one HD patients (mean age 59.3 ± 12.8 years) were included in our study. Waist circumference (WAC) was measured and abdominal obesity was defined according to the International Diabetes Federation. Serum levels of lipids (triglycerides, high density lipoproteins (HDL) cholesterol, low density lipoproteins (LDL) cholesterol) and inflammatory mediators (interleukin–6, tumor necrosis factor–alpha, vascular cellular adhesion molecule–1 (VCAM–1), intercellular adhesion molecule–1 (ICAM–1)) were measured. Patients were observed from the date of measurement (November 2003) of inflammatory mediators until their death or to 10th of November 2009.
Results: The mean WAC value for men was 97.6 ± 16.1 cm, and for women 92.2 ± 15.9 cm. Abdominal obesity was found in 62% of the enrolled patients. Cox regression analysis showed that the inflammatory mediators VCAM–1 (p<0.031) and ICAM–1 (p<0.024) were predictors of CV mortality in abdominal obese HD patients. Both inflammatory mediators remained predictors of CV mortality if age and other known risk factors for atherosclerosis (arterial hypertension, smoking, HDL and LDL cholesterol and triglycerides) were included in the analysis.
Conclusion: The results of our study indicate that microinflammation is associated with CV mortality in abdominal obese HD patients.
Downloads
Downloads
Published
Issue
Section
License
Copyright (c) 2013 Acta Medico-Biotechnica

This work is licensed under a Creative Commons Attribution 4.0 International License.